Sexual Wellness of Women: Desire, Pleasure, and Health in Real Life

Table of Contents
- Overview: What Sexual Wellness Actually Means for Women
- Mind–Body Connection: How Mood, Stress, and Depression Shape Female Desire
- Comfort, Arousal, and Orgasm: Why Sex Hurts or Feels Unsatisfying for Many Women
- Contraception, the Pull-Out Method, and What Really Protects Women’s Health
- Partners, Technique, and Shared Responsibility for Women’s Sexual Wellness
- Conclusion: Sexual Wellness of Women Is Ongoing, Not a One-Time Fix
- FAQ
Overview: What Sexual Wellness Actually Means for Women
Expert Insight: According to my.clevelandclinic.org, common penile conditions range from erectile dysfunction and skin diseases like herpes, syphilis, psoriasis, and eczema to emergencies such as paraphimosis, as well as penile cancer and penile fracture, all of which can impair urination, sexual function, or fertility (https://my.clevelandclinic.org/health/body/penis). (my.clevelandclinic.org)
Women’s sexual wellness is much more than whether sex “works” or leads to pregnancy. It includes desire, arousal, lubrication, comfort, orgasm, emotional connection, and a sense of safety and autonomy. Medical issues, mood, stress, relationship dynamics, and even misinformation about mens sexual wellness can all influence a woman’s experience in bed.
Healthy sexual function in women depends on:
- Physical factors like hormones, pelvic blood flow, nerve function, and vaginal tissue health.
- Mental and emotional health including depression, anxiety, trauma history, and body image.
- Relationship quality such as trust, communication, and whether a partner respects boundaries and feedback.
- Practical choices like contraception methods, STI prevention, and understanding how sex techniq can improve comfort and pleasure.
Sexual wellness is not one-size-fits-all. The goal is not constant high desire, but a sex life that feels chosen, safe, and satisfying—and that can change at different life stages without shame.
Mind–Body Connection: How Mood, Stress, and Depression Shape Female Desire
Every sexual sensation starts in the brain. When a woman experiences desire or feels emotionally close to a partner, the brain releases neurotransmitters that increase blood flow to the genitals and trigger arousal, swelling of the clitoris and vaginal walls, and lubrication. When depression or chronic stress is present, this signaling can be disrupted.
Depression and anxiety can affect women’s sexual wellness in several ways:
- Lower interest in sex: Low libido, trouble feeling mentally “switched on,” or sex feeling like a chore.
- Reduced physical response: Vaginal dryness, difficulty becoming or staying aroused, or delayed or absent orgasm.
- Less pleasure: Brain chemistry changes can blunt physical and emotional satisfaction even when sex is technically “working.”
Antidepressant medications can help mood but may also increase sexual side effects, including lower desire and difficulty reaching orgasm. These side effects are common and treatable; options can include dose adjustments, timing sex before a daily dose, or trying a different medication under medical guidance.
Partners often misinterpret these changes as rejection or lack of attraction. A more accurate frame is: the brain and body are under strain. Practical support includes:
- Normalizing mental health care as part of sexual wellness.
- Shifting pressure away from intercourse toward lower-stress touch, cuddling, or mutual massage.
- Checking in with simple questions like, “What would feel good or restful for you tonight?” instead of assuming sex is off or on.
When depression improves—through therapy, medication, lifestyle changes, or all three—women often report better libido, stronger arousal, and more satisfying orgasms. Treating mental health is a core sex techniq in itself.
Comfort, Arousal, and Orgasm: Why Sex Hurts or Feels Unsatisfying for Many Women
Many women tolerate pain, numbness, or low pleasure for years because they assume it is “normal” or that nothing can be done. In reality, most problems have specific causes and solutions.
Common reasons women don’t enjoy sex include:
- Insufficient arousal time: The body needs extended stimulation—often 15–30 minutes or more of kissing, oral sex, or manual touch—to fully lubricate and relax. Rushing to penetration increases pain, tearing, and resentment.
- Hormonal changes: After childbirth, during breastfeeding, and around menopause, estrogen shifts can thin vaginal tissues and reduce natural lubrication, causing burning or soreness during and after sex.
- Pelvic floor issues: Tight, overactive pelvic muscles can turn penetration into a painful or impossible experience. This can be linked to stress, trauma, chronic pain, or childbirth.
- Infections or skin conditions: Yeast infections, bacterial vaginosis, and inflammatory skin conditions can all make sex feel raw or stingy.
- Mismatch in technique: Many women need direct or indirect clitoral stimulation to reach orgasm. Penetration-focused routines often ignore this, leading to one-sided pleasure.
Practical steps to improve comfort and pleasure include:
- Reframing foreplay as “sex”, not just warm-up. Clitoral-focused touch, oral sex, and mutual masturbation are primary events, not optional extras.
- Using plenty of lubricant, especially during hormonal shifts or when using condoms. Water-based or silicone-based lubes can dramatically change comfort.
- Experimenting with angles and positions that reduce pressure on sensitive areas. Slow, shallow thrusting can feel better than deep, fast penetration.
- Prioritizing external stimulation for orgasm, with or without penetration. Most women do not orgasm from penetration alone, and that is normal anatomy, not a dysfunction.
- Seeking medical care if there is burning, bleeding, persistent pain, or sudden change in comfort—these are health signals, not things to “push through.”
Partners who are familiar with mens sexual wellness topics like ejaculation control, pacing, and arousal can use those same skills for women’s benefit: slowing down, reading feedback, and adjusting intensity to match her body instead of forcing a scripted routine.
Contraception, the Pull-Out Method, and What Really Protects Women’s Health
Contraception choices directly shape women’s sexual wellness. They influence pregnancy risk, STI risk, stress levels, and sometimes hormones and mood. One method that often gets misunderstood is withdrawal, or the “pull-out” method.
With withdrawal, a partner removes the penis from the vagina before ejaculation to avoid releasing semen inside. While it is better than no method at all, it has important limitations:
- Pre-ejaculate can contain sperm, especially if a man ejaculated earlier and did not urinate thoroughly afterward.
- It relies on perfect timing and control, which can fail during intense arousal, changing positions, or if a partner ejaculates sooner than expected.
- It offers zero protection against STIs because skin-to-skin contact, genital fluids, and microscopic tears can transmit infections long before ejaculation.
Safer, more reliable contraception options for women and couples include:
- Barrier methods such as condoms (external and internal), which protect against both pregnancy and most STIs when used correctly.
- Hormonal methods like pills, patches, rings, injections, or hormonal IUDs, which can dramatically reduce pregnancy risk but may affect mood or libido for some women.
- Non-hormonal options such as copper IUDs or fertility awareness, which require guidance and consistent tracking.
Withdrawal may still be part of a couple’s strategy, but it should be seen as a backup, not a primary method, especially where pregnancy would be high-risk or deeply unwanted. True sexual wellness for women includes the right to make informed decisions, to say no to “just pull out” if that does not feel safe, and to choose contraceptive methods that align with their health profile and life goals.
Men who invest in their own sexual health—whether learning better ejaculation control, addressing erectile issues, or smartly using tools like a penis extender or penis stretcher—should match that effort with equal responsibility for contraception and STI prevention, so the physical burden does not fall solely on women.
Partners, Technique, and Shared Responsibility for Women’s Sexual Wellness
Women’s sexual wellness does not exist in isolation. Partners’ habits, knowledge, and attitudes—especially around mens sexual wellness—strongly influence a woman’s experience of safety and pleasure.
Areas where male partners often need to level up include:
- Communication skills: Asking what feels good, listening when she says something hurts, and treating feedback as essential data, not criticism.
- Technique variety: Shifting focus away from rapid penetration and racing toward ejaculation, and toward slower build-up, teasing, clitoral focus, and pausing to let her arousal catch up.
- Body-awareness work: Men who practice better arousal control—through breath, pacing, or medically supervised techniques—tend to be more attentive lovers because they are not fighting their own climax from the first touch.
- Respect for boundaries: Accepting a no without sulking, and creating space for her to decline or change activities without fear of conflict.
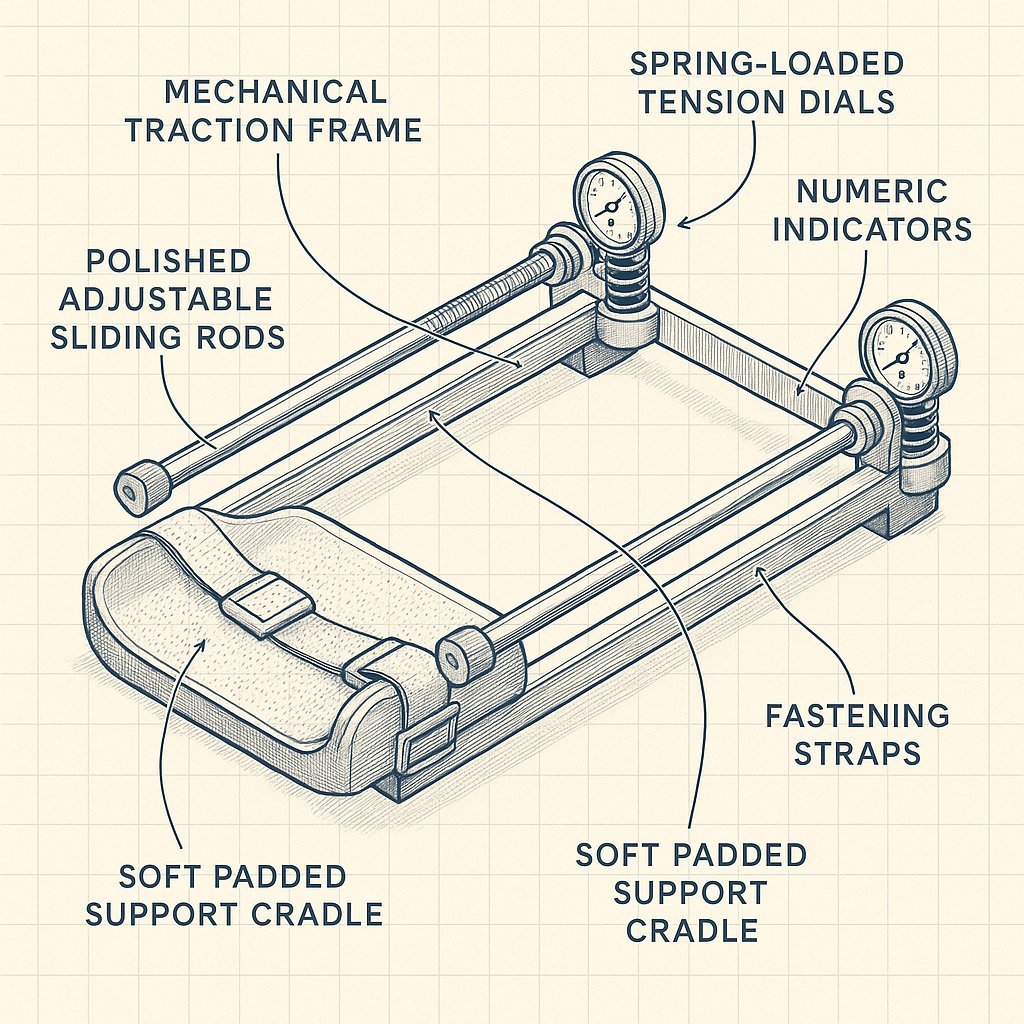
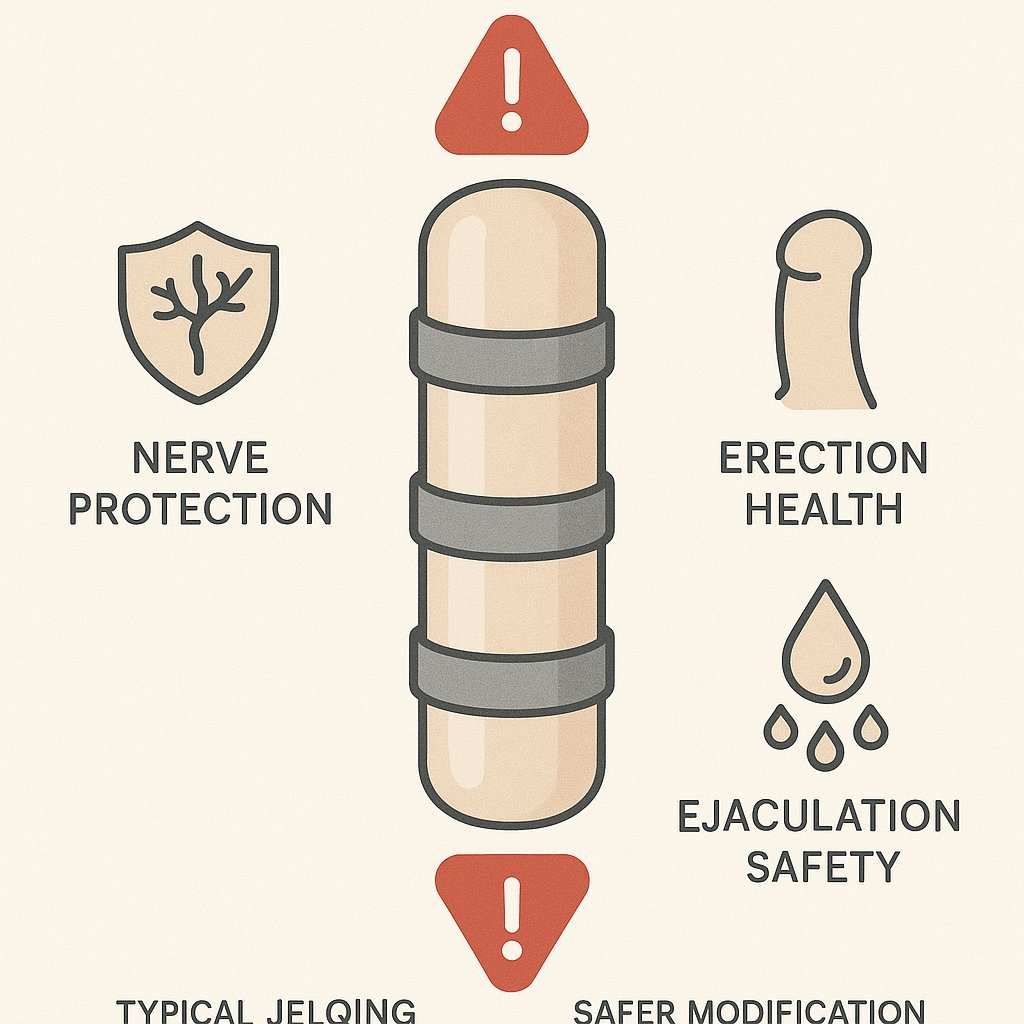
Some men explore enhancement methods such as jelq exercises, a penis extender, or a penis stretcher with the hope of improving confidence and performance. These tools should never replace core sex techniq like communication, emotional presence, and clitoral-focused stimulation, which matter far more to most women’s pleasure than size or hardness alone.
If a man chooses to experiment with hardware, safer design and medically oriented products are crucial. One example is the official PeniMaster store, which emphasizes clinically oriented traction devices; this kind of thoughtful approach is far more compatible with long-term sexual health—for both partners—than untested gadgets or dangerous DIY methods.
Ultimately, the most valuable “performance upgrade” for women’s sexual wellness is not equipment, but a partner who:
- Shows up with curiosity instead of ego.
- Values her comfort and orgasm as much as his own ejaculation.
- Understands that emotional safety is a powerful aphrodisiac.
When both partners share responsibility for education, contraception, and ongoing check-ins about what is working and what is not, women are far more likely to experience sex as something nourishing instead of draining.
Conclusion: Sexual Wellness of Women Is Ongoing, Not a One-Time Fix
Women’s sexual wellness is an evolving process shaped by age, hormones, mental health, relationships, and life stress. Desire will rise and fall; techniques that once worked may need updating; contraception needs can change. None of this means something is “wrong”—it means the system is alive.
The most sustainable approach is to treat sex as part of overall health, not a separate or shameful topic. That includes:
- Seeking medical care when pain, dryness, or sudden changes appear.
- Taking depression, anxiety, and trauma seriously as sexual health issues.
- Choosing contraceptive methods that feel safe and realistic for this season of life.
- Encouraging partners to invest in their own sexual education—about their bodies, ejaculation control, and safer enhancement tools—so the load is shared.
Women deserve sex lives that feel chosen, pleasurable, and respectful. That outcome depends as much on informed choices and supportive partners as on any hormone level or anatomy detail—and it is achievable at any age with the right mix of knowledge, care, and communication.
FAQ
Q: What factors influence a woman’s sexual desire?
A: Desire is shaped by hormones, mental health, stress levels, relationship dynamics, body image, and past experiences. It can naturally fluctuate over time, so noticing patterns and triggers helps you understand what supports or dampens your arousal.
Q: Why does sex sometimes feel painful or uncomfortable for women?
A: Pain can stem from insufficient arousal and lubrication, tension or anxiety, certain contraceptives, or underlying health conditions. Adjusting foreplay, using lubricant, and exploring different positions are practical first steps to reduce discomfort.
Q: How can partners communicate better about sexual needs and boundaries?
A: Choose low-pressure moments outside the bedroom to talk about what feels good, what doesn’t, and what you’d like to try. Using “I” statements, staying curious instead of critical, and agreeing to check in regularly builds trust and safety.
Q: How do contraception choices affect women’s sexual wellness?
A: Some contraceptives can influence libido, natural lubrication, or mood, while others may offer peace of mind that enhances enjoyment. Reviewing how a method makes you feel in daily life and during sex helps you decide whether it’s still the right fit.
Q: What practical steps can women take to improve sexual satisfaction?
A: Prioritizing sleep, stress management, and movement can boost energy and body confidence, which often improves sex. Exploring self-pleasure, using toys or lubricant, and being specific with partners about pace, pressure, and timing can directly increase pleasure.



Post Comment